The Doctors
George W. Rozakis, MD
Dr. Rozakis is a board certified biomedical engineer who studied
medicine at Cornell Medical Center and studied Ophthalmology at
the Duke Eye Center.
Dr. Rozakis worked in the field of Advanced Wellness / Functional
Medicine & The Optimization of Biochemistry for over 15 years. He has
applied this science age-related chronic conditions. Dr. Rozakis won
the advancements in healthcare award in Cleveland, Ohio (beating
out the Cleveland Clinic) in 2015 for his work in Advanced Wellness
and advocates for this approach to health care to his patients and
colleagues.
Dr. Rozakis pioneered the field of Lasik refractive surgery, phakic
refractive lenses, and the use of hormones and other advanced
testing to treat macular degeneration, migraine, parkinson's, arthritis,
insomnia, menopause, low testosterone, auto immune disease and
other age-related chronic conditions. He wrote a textbook on
refractive surgery and holds multiple patents. He was one of the first
surgeons in the world to perform LASIK. In 1998, he was voted by his
peers to receive an international award for his contributions to
LASIK refractive surgery. Dr. Rozakis published an extensive textbook on
refractive surgery that was read throughout the world and even
translated into Japanese.
Brian Bakke, Ph.D.
Dr. Bakke serves as a science advisor to the Advanced Program and
Macular Program. Dr. Bakke holds a PhD in bio-organic chemistry
and his thesis work focused on the development of DNA alkylating
agents for use as drug delivery systems. His post-doctoral work was
focused on the development of iso-adenosine analogues as
methylation pathway inhibitors for use as chemotherapeutic agents.
Dr. Bakke also holds a master’s degree in human nutrition from
Columbia University. His master’s thesis work focused on studying
the clinical nutrition practice patterns used by eye professionals in
the prevention and treatment of Age-Related Macular Degeneration
(AMD). In conjunction with his master's thesis work, Dr. Bakke
completed a 1-year clinical nutrition program for health
professionals through Columbia University Medical Center and the
Institute of Human Nutrition.
Prior to partnering with the Advanced Wellness Program through
Investihealth, Dr. Bakke spent 6 years working as chief science
officer with a medical consulting company. His work as chief science officer
focused on collaborating with primary care physicians in developing
personalized nutrition and bioidentical hormone based care plans
for improving clinical outcomes for patients with complex medical
conditions. Previously, Dr. Bakke spent 7 years working with the multi-
national chemistry, biotechnology and life science companies BASF
and Syngenta as a senior chemist.
George W. Rozakis, MD
Dr. Rozakis is a board certified biomedical engineer who studied
medicine at Cornell Medical Center and studied Ophthalmology at the Duke Eye Center.
Dr. Rozakis worked in the field of Advanced Wellness / Functional
Medicine & The Optimization of Biochemistry for over 15 years. He has
applied this science age-related chronic conditions. Dr. Rozakis won the advancements in healthcare award in Cleveland, Ohio (beating out the Cleveland Clinic) in 2015 for his work in Advanced Wellness and advocates for this approach to health care to his patients and colleagues.
Dr. Rozakis pioneered the field of Lasik refractive surgery, phakic refractive lenses, and the use of hormones and other advanced testing to treat macular degeneration, migraine, parkinson's, arthritis, insomnia, menopause, low testosterone, auto immune disease and other age-related chronic conditions. He wrote a textbook on refractive surgery and holds multiple patents. He was one of the first surgeons in the world to perform LASIK. In 1998, he was voted by his peers to receive an international award for his contributions to
LASIK refractive surgery. Dr. Rozakis published an extensive textbook on
refractive surgery that was read throughout the world and even
translated into Japanese.
Brian Bakke, Ph.D.
Dr. Bakke serves as a science advisor to the Advanced Program and Macular Program. Dr. Bakke holds a PhD in bio-organic chemistry and his thesis work focused on the development of DNA alkylating agents for use as drug delivery systems. His post-doctoral work was focused on the development of iso-adenosine analogues as
methylation pathway inhibitors for use as chemotherapeutic agents.
Dr. Bakke also holds a master’s degree in human nutrition from Columbia University. His master’s thesis work focused on studying the clinical nutrition practice patterns used by eye professionals in the prevention and treatment of Age-Related Macular Degeneration (AMD). In conjunction with his master's thesis work, Dr. Bakke
completed a 1-year clinical nutrition program for health professionals through Columbia University Medical Center and the Institute of Human Nutrition.
Prior to partnering with the Advanced Wellness Program through Investihealth, Dr. Bakke spent 6 years working as chief science officer with a medical consulting company. His work as chief science officer focused on collaborating with primary care physicians in developing personalized nutrition and bioidentical hormone based care plans for improving clinical outcomes for patients with complex medical conditions. Previously, Dr. Bakke spent 7 years working with the multi-national chemistry, biotechnology and life science companies BASF and Syngenta as a senior chemist.
The Science
The Optimization Of Body Chemistry - As applied to Macular
Degeneration as an example of an age-related condition. Keep in
mind this is the same process and thinking towards all chronic age-
related conditions...
A problem well stated is a problem half solved.
What is the problem with macular degeneration?
Let’s answer.
The problem that defines macular degeneration is sickness of the
retinal pigment epithelial cells (RPE).
These are important cells that sit underneath the photoreceptor cells
of the macula, which are the light-sensitive cells that allow for
vision.
Here are pictures of the retinal pigment epithelial (RPE) cells below
the photoreceptors rods and cones.
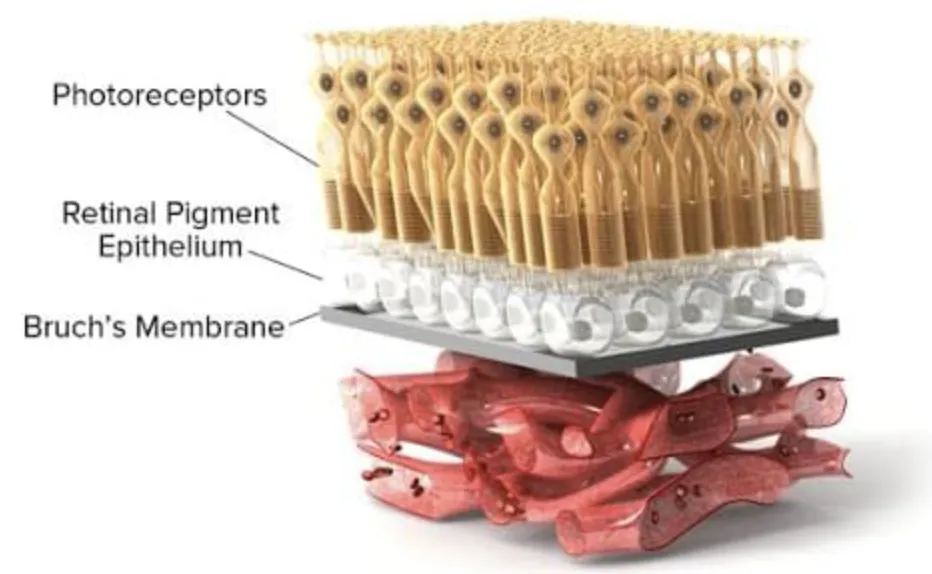
The retinal pigment epithelium (RPE) is a very active layer of cells.
The cell's role it is to keep the photoreceptors working correctly.
When the RPE cells start to deteriorate, vision declines.
So naturally, a possible pathway to prevention for macular
degeneration involves optimizing the health of these critical cells.
Does that make sense? It is worth repeating...
The possible pathway to preventing macular degeneration is
through optimizing the health of the RPE cells.
To make the RPE healthy we must know how those cells work. That is
the world of physiology. It includes everything that pertains to how
living organisms function.
The word for sickness is pathophysiology. Pathos is from the Greek
and means sickness.
So, what is the pathophysiology of the RPE in macular degeneration
and how are we able to improve the health of RPE cells?
The current guidelines for treating macular degeneration involves
the recommendation of the AREDS formulation that includes
vitamins and minerals such as Lutein, Zeaxanthin, Zinc, Vitamin C,
Vitamin E and Copper.
While the AREDS formulation may be beneficial in delaying blindness
for some, it falls short of being a solution. (In fact, AREDS only may
help 5.9% of patients. With Advanced Wellness, we are seeing time
and time again that we can do more.)
Improving the health of the RPE is much more complicated than that.
We now explain how to make the RPE cells healthier.
Before explaining our 20+ year clinical approach to macular
degeneration, there is an important point to be made regarding RPE
cells. Our approach to improving the health of RPE cells in your eye
applies to every cell in your body. All cells can benefit. Therefore,
when we improve the health of RPE cells, we are also improving the
health of cells throughout the body, which is why you will likely see
improvement in other symptoms and conditions. This approach can
be broadly viewed as anti-aging, functional medicine, natural
medicine or advanced wellness medicine.
YOUR PERSONALIZED CARE PLANS
The first phase of our approach is to utilize testing and a
comprehensive health historyevaluation to identify physiologic
factors that are contributing to your risk of macular degeneration
and other conditions that you may have or be at risk of acquiring.
The process begins with an evaluation of your health history.
Next, you will complete a comprehensive blood chemistry test panel.
We are especially interested in assessing your hormone levels as
hormone decline is associated with a number of age related health
risks for individuals over the age of 55. Hormone decline is an
unfortunate part of the aging process, and macular degeneration is
an age-related disease. We measure your hormones and
associated blood chemistry, identify deficiencies and recommend
the appropriate hormone replacement program to provide the
optimal levels of hormones to support healthy aging. Problem stated
problem solved.
Another blood test we recommend is a methylation biochemistry
test. Methylation is a crucial biochemical pathway in that directly
impacts the health of the cells in your body. Testing, identifying and
addressing methylation issues can help improve cellular health in a
number of ways. One key way that methylation can impact macular
degeneration is through the interaction of methylation pathway
biomolecules and the gene regulation of VEGF. VEGF is signaling
protein involved in the pathogenesis of wet macular degeneration.
Why methylation biochemistry and your hormones matter.
The methylation test also allows for the assessment of your degree
of oxidative stress and in turn, inflammation. Oxidative stress and
inflammation are key drivers of unhealthy aging and disease, which
includes macular degeneration.
Nutrition is another crucial driver of cellular health. We perform a
comprehensive review of your dietary patterns, nutritional genetic
risk factors and when indicated, food sensitivity testing. Our dietitians
will guide you through the process of implementing the dietary
modifications that will help improve the health of your RPE cells and
the other cells of your body.
The more data we have, the better we can define your care plan to
help improve your health.
What has our experience been with other patients?
When we first starting working with eye patients using this approach
over ten years ago, we were primarily focused on slowing down the
progression of macular degeneration.
To our delight, we began to receive feedback from patients that
included vision improvements when entering dark settings such as a
movie theater. As we all know, entering a dark movie theater is a
challenge for our eyes because we need to be able to switch from
bright light to low light. This is called dark adaptation. Today there
exists a test to detect early macular degeneration by examining dark
adaption.
The conventional approach to nutritional therapy (AREDS) for
slowing the progression of macular degeneration only slows vision
loss in 1 in 17 individuals. Unfortunately, this approach does not
improve vision and it does not prevent the disease from developing.
Much of what you have read up to now pertains to dry macular
degeneration. If you had asked me four years ago if we could help
wet macular degeneration I would have said no. Wet macular
degeneration is different than dry macular degeneration. Wet
macular degeneration involves the invasion of blood vessels through
the RPE and under the macula. It’s a very serious problem and is a
cause of severe vision loss and blindness. In the past, we would
apply a laser to the new blood vessels in an effort to save vision.
Unfortunately, the laser would also damage the macula, which
would cause blind spots.
We never anticipated that our advanced wellness approach would
help wet macular degeneration.
Until Pat.
Pat had wet macular degeneration and was being treated with the
current standard in wet macular degeneration care. Pat's
medications were injected into her eye every six weeks. These
injections lower VEGF levels in the eye, which in turn helps slow the
progression of the disease (and vision loss). The problem is that after
6 months of injections, the therapy was NOT working. Pat's wet
macular degeneration was progressing.
Pat enrolled in our program as a last resort, with little hope that her
advanced wellness program would help. But it did. Pat’s injections
started working, and after six months her eye health (and RPE cells)
improved so much that her retina doctor stopped giving her the
anti-VEGF injections. AMAZING. She is now four years out and has not
required an injection. Pat's amazing story was covered on a local
news station in Cleveland.
How were we able to help Pat convert from wet back to dry macular
degeneration? The short answer is that our program likely lowered
inflammation and VEGF in the eye.
That is the story behind the macular program. We look forward to
working with you to help improve the health of your eyes and your
body.
Start understanding what macular degeneration treatment and
overall health personalized care plan you need by Starting a Chat
With An Advisor. Secure. HIPAA Compliant.
The Optimization Of Body Chemistry - As applied to Macular Degeneration as an example of an age-related condition. Keep in mind this is the same process and thinking towards all chronic age-related conditions...
A problem well stated is a problem half solved.
What is the problem with macular degeneration?
Let’s answer.
The problem that defines macular degeneration is sickness of the
retinal pigment epithelial cells (RPE).
These are important cells that sit underneath the photoreceptor cells
of the macula, which are the light-sensitive cells that allow for
vision.
Here are pictures of the retinal pigment epithelial (RPE) cells below
the photoreceptors rods and cones.
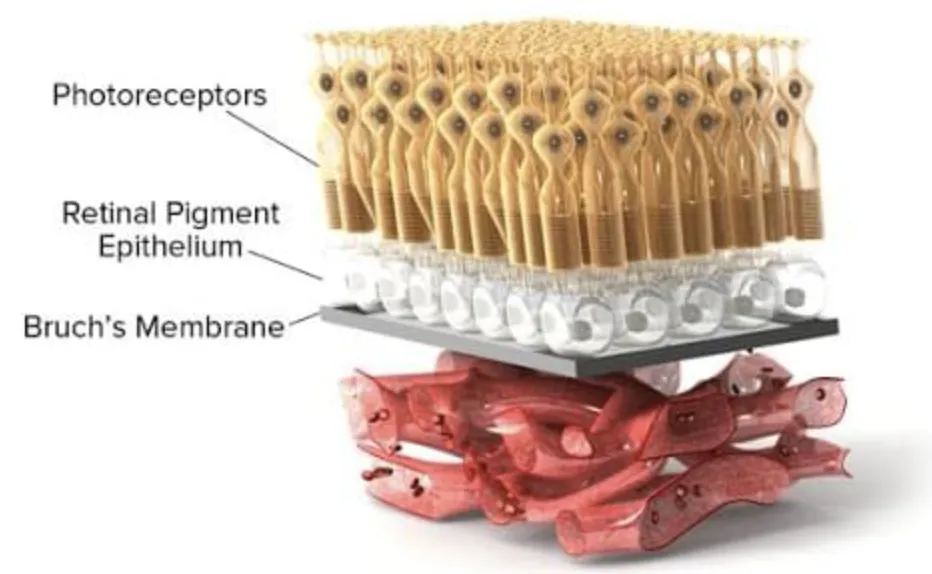
The retinal pigment epithelium (RPE) is a very active layer of cells. The cell's role it is to keep the photoreceptors working correctly. When the RPE cells start to deteriorate, vision declines.
So naturally, a possible pathway to prevention for macular degeneration involves optimizing the health of these critical cells.
Does that make sense? It is worth repeating...
The possible pathway to preventing macular degeneration is through optimizing the health of the RPE cells.
To make the RPE healthy we must know how those cells work. That is the world of physiology. It includes everything that pertains to how living organisms function.
The word for sickness is pathophysiology. Pathos is from the Greek and means sickness.
So, what is the pathophysiology of the RPE in macular degeneration and how are we able to improve the health of RPE cells?
The current guidelines for treating macular degeneration involves the recommendation of the AREDS formulation that includes vitamins and minerals such as Lutein, Zeaxanthin, Zinc, Vitamin C, Vitamin E and Copper.
While the AREDS formulation may be beneficial in delaying blindness for some, it falls short of being a solution. (In fact, AREDS only may help 5.9% of patients. With Advanced Wellness, we are seeing time and time again that we can do more.)
Improving the health of the RPE is much more complicated than that.
We now explain how to make the RPE cells healthier.
Before explaining our 20+ year clinical approach to macular degeneration, there is an important point to be made regarding RPE cells. Our approach to improving the health of RPE cells in your eye applies to every cell in your body. All cells can benefit. Therefore, when we improve the health of RPE cells, we are also improving the health of cells throughout the body, which is why you will likely see improvement in other symptoms and conditions. This approach can be broadly viewed as anti-aging, functional medicine, natural
medicine or advanced wellness medicine.
YOUR PERSONALIZED CARE PLANS
The first phase of our approach is to utilize testing and a comprehensive health historyevaluation to identify physiologic
factors that are contributing to your risk of macular degeneration and other conditions that you may have or be at risk of acquiring.
The process begins with an evaluation of your health history.
Next, you will complete a comprehensive blood chemistry test panel. We are especially interested in assessing your hormone levels as
hormone decline is associated with a number of age related health risks for individuals over the age of 55. Hormone decline is an unfortunate part of the aging process, and macular degeneration is an age-related disease. We measure your hormones and associated blood chemistry, identify deficiencies and recommend
the appropriate hormone replacement program to provide the optimal levels of hormones to support healthy aging. Problem stated problem solved.
Another blood test we recommend is a methylation biochemistry test. Methylation is a crucial biochemical pathway in that directly impacts the health of the cells in your body. Testing, identifying and addressing methylation issues can help improve cellular health in a number of ways. One key way that methylation can impact macular
degeneration is through the interaction of methylation pathway biomolecules and the gene regulation of VEGF. VEGF is signaling protein involved in the pathogenesis of wet macular degeneration.
Why methylatio biochemistry and your hormones matter.
The methylation test also allows for the assessment of your degree of oxidative stress and in turn, inflammation. Oxidative stress and inflammation are key drivers of unhealthy aging and disease, which includes macular degeneration.
Nutrition is another crucial driver of cellular health. We perform a
comprehensive review of your dietary patterns, nutritional genetic risk factors and when indicated, food sensitivity testing. Our dietitians will guide you through the process of implementing the dietary modifications that will help improve the health of your RPE cells and
the other cells of your body.
The more data we have, the better we can define your care plan to help improve your health.
What has our experience been with other patients?
When we first starting working with eye patients using this approach over ten years ago, we were primarily focused on slowing down the progression of macular degeneration.
To our delight, we began to receive feedback from patients that included vision improvements when entering dark settings such as a movie theater. As we all know, entering a dark movie theater is a challenge for our eyes because we need to be able to switch from bright light to low light. This is called dark adaptation. Today there
exists a test to detect early macular degeneration by examining dark
adaption.
The conventional approach to nutritional therapy (AREDS) for slowing the progression of macular degeneration only slows vision loss in 1 in 17 individuals. Unfortunately, this approach does not improve vision and it does not prevent the disease from developing.
Much of what you have read up to now pertains to dry macular degeneration. If you had asked me four years ago if we could help wet macular degeneration I would have said no. Wet macular degeneration is different than dry macular degeneration. Wet
macular degeneration involves the invasion of blood vessels through the RPE and under the macula. It’s a very serious problem and is a cause of severe vision loss and blindness. In the past, we would apply a laser to the new blood vessels in an effort to save vision.
Unfortunately, the laser would also damage the macula, which would cause blind spots.
We never anticipated that our advanced wellness approach would
help wet macular degeneration.
Until Pat.
Pat had wet macular degeneration and was being treated with the current standard in wet macular degeneration care. Pat's medications were injected into her eye every six weeks. These
injections lower VEGF levels in the eye, which in turn helps slow the
progression of the disease (and vision loss). The problem is that after months of injections, the therapy was NOT working. Pat's wet macular degeneration was progressing.
Pat enrolled in our program as a last resort, with little hope that her advanced wellness program would help. But it did. Pat’s injections started working, and after six months her eye health (and RPE cells) improved so much that her retina doctor stopped giving her the anti-VEGF injections. AMAZING. She is now four years out and has not required an injection. Pat's amazing story was covered on a local
news station in Cleveland.
How were we able to help Pat convert from wet back to dry macular
degeneration? The short answer is that our program likely lowered
inflammation and VEGF in the eye.
That is the story behind the macular program. We look forward to working with you to help improve the health of your eyes and your body.
Start understanding what macular degeneration treatment and overall health personalized care plan you need by Starting a Chat With An Advisor. Secure. HIPAA Compliant.